Introduction to Appendicitis and COVID-19
Appendicitis and COVID-19 are two medical conditions that, at first glance, seem completely unrelated. Appendicitis, an inflammation of the appendix, is a common surgical emergency, while COVID-19 is a respiratory illness caused by the novel coronavirus SARS-CoV-2. However, over the course of the pandemic, healthcare professionals and researchers have noticed intriguing interactions between these two conditions. Understanding how appendicitis and COVID-19 intersect is important for patients, caregivers, and medical staff alike, as it impacts diagnosis, treatment strategies, and outcomes.
Since the start of the COVID-19 pandemic, hospitals and emergency rooms worldwide have faced new challenges. Many people with appendicitis delayed seeking care due to fears of contracting COVID-19, and in some cases, COVID-19 itself complicated diagnosis and treatment of abdominal pain. This article will explore appendicitis and COVID-19 in detail, examining symptoms, diagnosis, treatment, and what the latest research tells us about their connection. We aim to provide a clear, engaging, and comprehensive overview for anyone interested or affected.
What is Appendicitis?
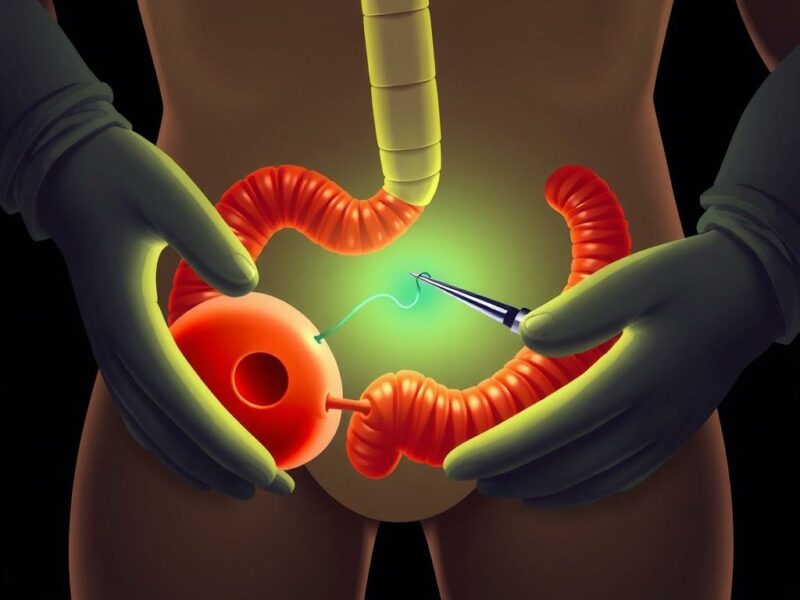
Appendicitis occurs when the appendix, a small tube-shaped pouch attached to the large intestine, becomes inflamed and infected. Though its precise function is not fully understood, the appendix can cause severe problems when blocked or irritated. The blockage often results from mucus, stool, or swelling of lymphoid tissue. Once blocked, the appendix can rapidly swell, leading to pain, infection, and potentially dangerous complications like rupture.
Symptoms of appendicitis typically start with abdominal discomfort around the belly button, gradually moving to the lower right side of the abdomen. This pain intensifies over time and is often accompanied by nausea, vomiting, loss of appetite, and fever. If untreated, the appendix can burst, spreading infection throughout the abdomen, which becomes a life-threatening condition called peritonitis. Quick diagnosis and intervention are crucial to prevent serious outcomes.
Common Symptoms of Appendicitis
- Abdominal pain, starting around the navel and shifting to the lower right side
- Nausea and vomiting
- Loss of appetite
- Fever and chills
- Constipation or diarrhea
- Abdominal swelling or bloating
Appendicitis requires prompt medical attention. Treatment often involves surgical removal of the appendix (appendectomy), although in some cases antibiotics may be tried first.
How COVID-19 Has Changed Healthcare for Appendicitis Patients

The COVID-19 pandemic disrupted healthcare systems worldwide, significantly affecting how appendicitis is managed. Many patients delayed or avoided going to emergency departments due to fear of catching the virus. This delay resulted in more cases of complicated appendicitis, with higher rates of appendix rupture and infection.
Hospitals also adapted their protocols to reduce COVID-19 transmission risk during surgeries. Non-operative management with antibiotics became a more favorable approach in select cases, especially when surgical resources were limited or the risk of COVID-19 exposure was high. Moreover, healthcare workers needed to distinguish symptoms caused by COVID-19 from those related to appendicitis, which sometimes overlapped or obscured the diagnosis.
The Impact of Delays in Appendicitis Treatment During COVID-19
| Factor | Impact |
|---|---|
| Fear of contracting COVID-19 | Patients delayed emergency visits |
| Reduced hospital capacity | Longer wait times and limited surgical slots |
| Preference for non-operative management | Increased use of antibiotics as initial treatment |
| Lack of clear symptoms differentiation | Misdiagnosis or late diagnosis of appendicitis |
This table summarizes some major challenges in managing appendicitis during the pandemic and highlights why understanding appendicitis and COVID-19 together is so vital.
Can COVID-19 Cause Appendicitis?
One of the key questions emerging in medical circles is whether COVID-19 can directly cause appendicitis. Several case reports and small studies suggest a possible association, especially in children and young adults. COVID-19 is known to trigger an intense immune response, inflammation, and sometimes gastrointestinal symptoms, which can mimic or even provoke appendicitis-like conditions.
The theory is that the viral infection may cause lymphoid hyperplasia (enlargement of lymphatic tissue) in the appendix, leading to obstruction and inflammation. Additionally, COVID-19-related blood clotting abnormalities and systemic inflammation could contribute to appendiceal ischemia or swelling. However, the evidence remains limited, and whether COVID-19 truly causes appendicitis or simply mimics its symptoms is still under investigation.
Signs That COVID-19 May Be Linked to Appendicitis Cases
- Increase in pediatric appendicitis cases with concurrent or recent COVID-19 infection
- Presence of unusual inflammatory markers in appendicitis patients during the pandemic
- Reports of appendiceal inflammation without bacterial infection in COVID-19 positive patients
- Prolonged or atypical abdominal symptoms in patients diagnosed with COVID-19
Still, most patients with appendicitis do not have COVID-19, and most COVID-19 patients do not develop appendicitis. This overlap is uncommon but has drawn attention as a potential area for closer monitoring, especially in emergency settings.
Diagnosing Appendicitis During the COVID-19 Pandemic
Diagnosing appendicitis is challenging even in the best of times, with symptoms that can overlap with many other conditions. The addition of COVID-19 complicates this further, as patients might present with diverse symptoms, including fever, abdominal pain, and gastrointestinal upset.
Healthcare providers often use a combination of clinical evaluation, blood tests (like white blood cell count), imaging (ultrasound or CT scans), and COVID-19 testing to get an accurate diagnosis. Rapid and comprehensive testing for COVID-19 has become standard practice before surgery, to protect both patients and staff.
Diagnostic Tools and Procedures
| Test/Procedure | Purpose | Considerations with COVID-19 |
|---|---|---|
| Physical examination | Assess abdominal tenderness and pain | May be hindered by infection control measures |
| Complete blood count (CBC) | Detects elevated white blood cells | Increased WBC can also occur with COVID-19 inflammation |
| Ultrasound | Non-invasive imaging of the appendix | Avoids radiation; good for children and pregnant women |
| CT scan | High accuracy imaging for appendicitis | Requires patient to enter hospital, risk of COVID-19 exposure |
| COVID-19 PCR or rapid antigen test | Confirm presence of coronavirus infection | Essential before surgical intervention |
Making the right call quickly is crucial to prevent complications. Collaboration and communication between surgical teams, infectious disease specialists, and emergency staff are key in managing these patients effectively.
Treatment Options: Surgery, Antibiotics, and Beyond

Traditionally, appendicitis treatment involves surgery—removing the inflamed appendix as soon as possible. The operation can be done as an open appendectomy or more commonly as a minimally invasive laparoscopic procedure. Surgery rapidly resolves the problem and prevents rupture.
However, during the COVID-19 pandemic, several factors shifted the approach to treating appendicitis. Hospitals facing resource limitations or COVID-19 outbreaks sometimes opted to treat uncomplicated appendicitis cases with antibiotics first. This approach reduces the need for surgery and hospital stays, potentially lowering COVID-19 exposure risk.
Comparing Appendicitis Treatment Approaches
| Treatment | Benefits | Drawbacks |
|---|---|---|
| Appendectomy (Surgery) | Definitive resolution; low chance of recurrence | Requires anesthesia; risk of COVID-19 exposure; longer hospital stay |
| Antibiotic Therapy | Non-invasive; can be administered outpatient | Risk of recurrence; may delay surgery if condition worsens |
| Watchful Waiting | Avoids unnecessary intervention | Potential progression to rupture; requires close monitoring |
Patients with complicated appendicitis (rupture, abscess) generally require surgery and sometimes drainage procedures. For COVID-19 positive patients needing surgery, special precautions are taken to prevent virus transmission, including negative pressure operating rooms and full protective equipment.
Special Considerations: Pediatric and Elderly Patients
Children and older adults present unique challenges when appendicitis and COVID-19 intersect. Pediatric patients often show varied symptoms of both conditions, and COVID-19 infection in children can lead to Multisystem Inflammatory Syndrome in Children (MIS-C), a serious condition that affects multiple organs including the gastrointestinal tract.
Elderly patients are at higher risk of severe COVID-19 and may have atypical symptoms of appendicitis, such as less localized pain or confusion. Delays in diagnosis and treatment in these age groups can lead to higher complication rates.
Healthcare providers must take account of these factors, applying tailored diagnostic and treatment approaches to improve outcomes.
Vaccination and Prevention: What It Means for Appendicitis Patients
An important aspect of navigating appendicitis and COVID-19 is vaccination. While vaccines do not prevent appendicitis, they reduce the risk of severe COVID-19 infection and hospital transmission risks. For patients undergoing surgery, being vaccinated can decrease the likelihood of perioperative complications related to COVID-19.
Hospitals encourage vaccination among surgical candidates and medical staff to create safer environments. Patients diagnosed with appendicitis during the pandemic are advised to discuss vaccination status with their doctors, especially if surgery is planned.
Research and Emerging Insights
Ongoing research is shedding light on the complex relationship between appendicitis and COVID-19. Studies are focusing on how the virus’s inflammatory effects may trigger or mimic appendicitis, as well as evaluating the best treatment protocols in a pandemic context.
Some intriguing findings include:
- Increased incidence of appendicitis in children with recent COVID-19 infection
- Effectiveness of non-operative management when surgery is delayed due to COVID-19
- Identification of inflammatory markers that differentiate appendicitis from COVID-19 abdominal symptoms
- Long-term follow-up outcomes for patients treated with antibiotics alone during the pandemic
As more data accumulates, medical guidelines will continue to evolve, improving patient care and safety.
Tips for Patients: Recognizing Symptoms and Seeking Care
If you or a loved one experience abdominal pain, especially localized to the lower right side, don’t delay seeking medical attention. Remember that timely treatment of appendicitis is critical to avoiding serious complications. Here are some practical tips:
- Monitor symptoms closely, including fever, nausea, and abdominal tenderness
- Inform healthcare providers about any recent COVID-19 exposure or infection
- Ask about COVID-19 testing and safety protocols at your hospital or clinic
- Discuss vaccination status when planning any surgery or hospitalization
- Don’t assume abdominal pain is “just COVID-19”—get a thorough evaluation
Healthcare professionals are trained to balance risks and provide safe care even amid the pandemic, so prompt consultation can save lives.
Summary Table: Key Points on Appendicitis and COVID-19
| Topic | Key Information |
|---|---|
| Appendicitis Symptoms | Lower right abdominal pain, fever, nausea |
| COVID-19 Symptoms Overlap | Fever, gastrointestinal upset, abdominal discomfort |
| Diagnosis Challenges | Mimicking symptoms complicate diagnosis during pandemic |
| Treatment Adjustments | Increased use of antibiotics; precautionary surgery protocols |
| Patient Delays | Fear of COVID-19 causes treatment delays, worsening outcomes |
| Research Focus | Investigating COVID-19’s role in appendicitis onset and management |
Conclusion
In the intertwined story of appendicitis and COVID-19, understanding the nuances has never been more important. While appendicitis remains a common and urgent surgical condition, the pandemic introduced new challenges in diagnosis, treatment, and patient behavior. Delays in seeking care during COVID-19 surges have led to more complicated appendicitis cases, underscoring the importance of timely medical attention. The possibility that COVID-19 may contribute to or mimic appendicitis highlights the need for careful clinical evaluation. Treatment strategies have evolved, balancing the risks of surgery and infection with the benefits of minimally invasive procedures and antibiotic therapy. Special populations, such as children and elderly patients, require extra vigilance. With ongoing research, vaccination efforts, and improved healthcare protocols, managing appendicitis in the era of COVID-19 is becoming safer and more effective. If you ever face abdominal pain or symptoms suggestive of appendicitis, don’t hesitate to seek medical attention promptly—early intervention saves lives and helps navigate these challenging times with confidence.



