Appendicitis is one of the most common causes of acute abdominal pain requiring surgical intervention, but it is often a tricky diagnosis due to its overlapping symptoms with many other conditions. When a patient presents with right lower quadrant pain, fever, and nausea, healthcare providers must carefully consider a broad differential diagnosis to avoid misdiagnosis and unnecessary surgery. This article will guide you step-by-step through the differential diagnosis of appendicitis, exploring similar clinical presentations, key diagnostic tools, and how to distinguish between various conditions that mimic appendicitis.
Understanding Appendicitis and Its Importance
Appendicitis is the inflammation of the appendix, a small tube attached to the cecum in the large intestine. It typically presents with abdominal pain that starts around the navel and then shifts to the right lower quadrant (RLQ), accompanied by symptoms like nausea, vomiting, and low-grade fever. The condition often requires urgent surgical removal of the appendix to prevent rupture and subsequent complications like peritonitis and sepsis.
However, the challenge lies in that many other conditions can imitate these symptoms—causing abdominal pain in the same region or presenting with similar systemic signs. Misdiagnosing appendicitis can either lead to unnecessary appendectomy or delayed treatment of serious alternative causes. Therefore, understanding the differential diagnosis of appendicitis is critical for clinicians and students alike.
Common Conditions Mimicking Appendicitis
When approaching the differential diagnosis of appendicitis, physicians consider a wide spectrum of gastrointestinal, genitourinary, and gynecological disorders. Let’s explore these common conditions and how they can visually or symptomatically overlap with appendicitis.
Gastrointestinal Causes
- Mesenteric adenitis: Common in children and adolescents, it causes lymph node inflammation in the mesentery and can present with RLQ pain similar to appendicitis.
- Gastroenteritis: Infections of the gastrointestinal tract may produce diffuse abdominal pain and vomiting mimicking early appendicitis.
- Meckel’s diverticulitis: Inflammation of a Meckel’s diverticulum, an embryologic intestinal remnant, can resemble appendicitis clinically.
- Intestinal obstruction: Conditions causing bowel obstruction can cause localized pain, distention, and vomiting that overlap with appendicitis symptoms.
Gynecological Causes
In women of reproductive age, gynecologic conditions are commonly mistaken for appendicitis due to the proximity of pelvic organs to the appendix.
- Ovarian cyst rupture or torsion: Both can cause sudden, severe lower abdominal pain with nausea and vomiting.
- Ectopic pregnancy: A life-threatening condition requiring urgent diagnosis, ectopic pregnancy can cause RLQ pain and bleeding just like appendicitis.
- Pelvic inflammatory disease (PID): Infection of the upper genital tract manifests with lower abdominal pain and fever.
Urinary Causes
Urinary tract infections and kidney stones may also present with RLQ or flank pain, making them important differential diagnoses.
- Ureteric stone: Severe flank pain radiating towards the groin may mimic appendicitis pain distribution.
- Urinary tract infection (UTI): Dysuria, fever, and lower abdominal discomfort can sometimes be confused with appendicitis.
Other Conditions
- Right-sided diverticulitis: Though less common than left-sided diverticulitis, inflammation of the right colon segment can simulate appendicitis.
- Inflammatory bowel disease (Crohn’s disease): Inflammation in the terminal ileum can mimic appendicitis symptoms.
- Abdominal wall pathology: Muscle strain or hernias in the RLQ region can cause localized tenderness.
Symptoms and Signs: Clues for Differential Diagnosis
Many of the differential diagnoses discussed share a common clinical presentation—abdominal pain and systemic symptoms—but subtle differences exist. A thorough history and physical examination remain the mainstays in guiding diagnosis.
Characteristic Features of Appendicitis
Appendicitis typically begins with vague periumbilical pain, then localizes to the RLQ (McBurney’s point) within 12-24 hours. Patients often experience anorexia, nausea, vomiting, and low-grade fever. Abdominal guarding and rebound tenderness on examination may suggest peritoneal irritation.
Differentiating Factors in Mimicking Conditions
| Condition | Typical Symptoms | Physical Exam Clues | Additional Notes |
|---|---|---|---|
| Mesenteric adenitis | RLQ pain, often preceded by an upper respiratory infection | Tender lymphadenopathy in RLQ, less severe guarding | Common in children; often self-limiting |
| Ovarian torsion | Sudden severe lower abdominal pain, often unilateral | Adnexal tenderness, absent or decreased bowel sounds | Gynecologic ultrasound critical for diagnosis |
| Ectopic pregnancy | RLQ pain with vaginal bleeding, amenorrhea | Pelvic tenderness; positive pregnancy test | Life-threatening; must rule out with β-hCG test |
| Ureteric stone | Severe flank and groin pain, hematuria | Costovertebral angle tenderness | Imaging (CT) helps confirm diagnosis |
| Pelvic inflammatory disease | Lower abdominal pain, fever, vaginal discharge | Cervical motion tenderness, adnexal tenderness | Sexual history important; treat with antibiotics |
Diagnostic Tools in the Differential Diagnosis of Appendicitis
While clinical skills are paramount, diagnostic imaging and laboratory tests provide valuable assistance in narrowing down the diagnosis.
Laboratory Investigations
Basic labs include complete blood count (CBC), inflammatory markers (CRP), urinalysis, pregnancy test in females, and sometimes stool studies. Appendicitis typically shows leukocytosis with neutrophilia and elevated CRP, but these markers can also be elevated in other inflammatory or infectious conditions.
Imaging Modalities
- Ultrasound: First-line in children and pregnant women due to lack of radiation. Can detect an enlarged, non-compressible appendix, ovarian pathology, or free fluid.
- Computed Tomography (CT): The gold standard for adult appendicitis diagnosis due to high sensitivity and specificity. CT can also provide visualization of alternative diagnoses such as diverticulitis or renal stones.
- MRI: Useful in pregnancy or when radiation should be avoided, with good imaging of pelvic organs.
Scoring Systems to Aid Diagnosis
Several scoring systems help predict the likelihood of appendicitis based on clinical and lab findings:
| Score | Parameters | Purpose |
|---|---|---|
| Alvarado Score | Symptoms, signs, lab values (e.g., migration of pain, anorexia, leukocytosis) | Identifies risk of appendicitis; guides imaging needs |
| Pediatric Appendicitis Score | Similar parameters adapted for children | Aids diagnosis in pediatric patients |
Stepwise Approach to Diagnosing Appendicitis and Its Mimickers
Managing a patient with suspected appendicitis requires a systematic evaluation to consider differential diagnoses thoughtfully.
- Apply a detailed clinical history. Ask about onset, location, radiation, and progression of pain; associated symptoms such as fever, vomiting, diarrhea, urinary symptoms, or gynecologic history.
- Perform a thorough physical examination. Evaluate abdominal tenderness, peritoneal signs, and perform pelvic and rectal exams if indicated.
- Order baseline laboratory tests. CBC, CRP, urinalysis, and β-hCG in females of childbearing age.
- Use imaging based on risk assessment. Begin with ultrasound in children/pregnant patients or if ovarian pathology suspected; CT is preferred in adults if diagnosis is uncertain.
- Consider alternative diagnoses. If imaging and labs do not support appendicitis, evaluate for other conditions such as ovarian torsion, ectopic pregnancy, or urinary tract issues.
- Consult specialists when needed. Gynecologists, urologists, or surgeons can provide directed expertise for complex or uncertain cases.
Key Challenges in Diagnosing Appendicitis
Despite advances, many challenges persist in accurately diagnosing appendicitis. Atypical presentations, particularly in children, elderly, pregnant women, and immunocompromised patients, complicate clinical assessment. Additionally, early appendicitis may lack localized signs, while other conditions may cause similar inflammatory responses. The risk of both missed appendicitis and negative appendectomy pushes physicians to rely on a combination of clinical judgment, scoring systems, and targeted imaging studies.
Population-Specific Considerations
- Children: Abdominal pain localization is difficult; mesenteric adenitis is often more common than appendicitis.
- Pregnant women: The appendix is displaced; pain can present atypically.
- Elderly: Symptoms may be subtle or atypical, increasing risk of delayed diagnosis.
Summary Table of Differential Diagnosis Features
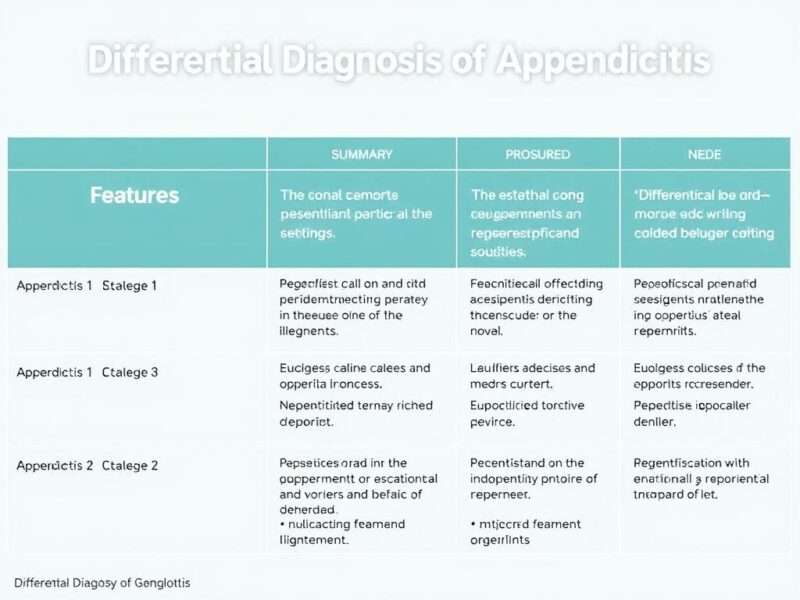
| Condition | Pain Location | Onset | Associated Symptoms | Imaging Modality |
|---|---|---|---|---|
| Appendicitis | RLQ, periumbilical migrating to RLQ | Gradual over hours | Nausea, vomiting, fever, anorexia | Ultrasound, CT |
| Ovarian torsion | Lower abdomen/pelvis, unilateral | Sudden onset | Nausea, vomiting, no fever | Pelvic ultrasound |
| Ectopic pregnancy | Lower abdomen, unilateral or bilateral | Variable | Vaginal bleeding, amenorrhea | Pelvic ultrasound, β-hCG |
| Mesenteric adenitis | RLQ | Gradual, often post-viral | Upper respiratory symptoms | Ultrasound |
When to Refer and When to Operate

The decision to operate is based on confirmed or highly suspected appendicitis. However, equivocal cases may warrant observation with serial examinations or further imaging to monitor progression. Referral to surgery should be prompt when signs of peritonitis or worsening clinical condition appear. Conversely, nonsurgical conditions like ovarian cysts or PID require specialist input and medical management.
Future Directions and Advances in Diagnosis
Emerging technologies such as point-of-care ultrasound, biomarkers, and improved imaging techniques aim to reduce diagnostic uncertainty. Artificial intelligence models and machine learning are also being explored to improve preoperative diagnostic accuracy and patient outcomes. Ultimately, a combination of clinical intuition supported by advanced diagnostics will shape the future approach to differentiating appendicitis from its mimickers.
Conclusion
Differential diagnosis of appendicitis is a complex but essential skill that requires integrating clinical history, physical examination, laboratory tests, and imaging studies to avoid pitfalls. Conditions ranging from gynecologic emergencies to urinary tract diseases may mimic appendicitis, making careful evaluation critical. Understanding the subtle nuances in presentation and applying a systematic approach helps ensure accurate diagnosis, timely treatment, and optimal patient outcomes. Whether you are a medical student, resident, or practicing clinician, mastering this diagnostic challenge is fundamental to providing excellent care in patients with acute abdominal pain.



